EFFECTIVENESS OF PREHABILITATION ON POST-OPERATIVE FUNCTIONAL OUTCOMES
Prehabilitation describes an intervention which aims to optimize physical functionality prior to surgery, enabling an individual to achieve a normal level of function quicker post operatively. The current evidence suggests structured progressive exercise, in combination with patient education will reduce pain and improve function pre and post-surgery.
- 150 minutes of Moderate-high intensity per week or 30 – 60 minutes of moderate-high intensity exercise 5 days/week. Once continuous session or multiple shorter sessions of 10 minutes are both acceptable to accumulate desired daily amounts of exercise.
+
- Progressive Strength Training 2-3 days/week at a moderate intensity.
+
- Stretching/Mobility exercises minimum 2-3 days/ week to improve and maintain range of motion.
+
- Neuromotor exercise or “functional exercise training” minimum 2-3 days/week to improve functional capacity, proprioception and balance, coordination and gait.
Shockingly, over a one week period 40% of adults with lower limb conditions do not engage in one session of moderate physical activity lasting 10 minutes.
Osteoarthritis (OA) is among the most prevalent chronic conditions and leading cause of joint pain and disability in older adults. OA of the peripheral joints including knees and hip are associated with progressive decline in strength, mobility, functional capacity and overall quality of life. Reduced lower body strength and stability predispose older adults to falls and effectively reduces an individual’s ability to perform functional tasks. Individuals with knee OA often present with significantly lower quadriceps strength and associated muscle wasting in a comparison between non-affected limbs or age-matched comparisons.
Patients will experience up to 50% improvement in pain by reducing body weight by just 10%. A combination of progressive strength, mobility, functional training and aerobic exercises are important as both muscle strength and cardiovascular capacity declines post-operatively.
Influence of Progressive Loading on Joint Integrity
Muscles and joints are intended to tolerate and adapt to load. Adaptation to load allows structures including muscles, cartilage and ligaments to maintain their integrity, function and reduction in pain levels. Degeneration of articular cartilage and joint integrity are often attributed to multiple risk factors including:
- Joint Stability
- Malalignment
- Obesity
- History of Joint Injury
- Associated muscle weakness or dysfunction
- Age
- Genetics
Rate of degeneration in conditions including Osteoarthritis are influenced by factors including functional capacity, physical inactivity, lifestyle and behavioural factors.
Effective management of joint function and integrity needs to consider the global needs of an individual to overcome the existing symptoms, including physical, social and psychological factors. Such factors have an effect on their overall quality of life, ability to complete activities of daily living, employment capacity, family commitments and leisure activities.
Severity of joint degeneration is directly related to decrease in muscular strength and altered joint biomechanics. Chronic joint pain contributes to anxiety, depression, fear of movement and poor physiological outlook. A fear of movement commonly affects individuals from participating in exercise as a result of fear of exacerbating symptoms or degeneration. Evidence suggests that up to 10,000 steps per day of activity does no accelerate progression of joint degeneration.
Aerobic Exercise and Post-Operative Outcomes
Cardiovascular fitness is a strong predictor of mortality. In response to exercise the body increases in cardiac output and efficiency of oxygen delivery, directly impacting skeletal muscle function. Muscle adaptation to exercise increases mitochondrial content and oxygen uptake capacity. Increased cell energy content and improved oxygen uptake directly influences the muscle ability to develop force through strength and ability to adapt to varying loads. Overall, improving the body’s functional reserves allows the individual to meet the metabolic demands of surgery and the post-operative period. The body’s normal response to surgical stress will see changes in the neuroendocrine, metabolic and immune systems, experienced as an amplification of the “fight or flight reaction”. Changes produce an increase in oxygen consumption, metabolic rate, protein breakdown and nitrogen balance.
Progressive Strength Exercise in Pre & Post-Operative Outcomes
Periods of prolonged relative inactivity or reduced joint movement (e.g. braces) during the recovery period will elicit a degree of deconditioning with muscle atrophy, loss of contractibility and strength.
Impaired muscle strength, gait speed, agility and dynamic balance are common predictors of delayed post-operative functional recovery. 20% of patients reported worse or no improvements in pain post-surgery. Poor physical function prior to surgery is a pre-cursor for a further decline in physical function and increased period of hospitalisation. The impact of surgery elicits a 20-40% reduction in post-operative physical function without the added incapacity of poor physical function prior to surgery. Evidently, the effects of Prehabilitation prior to surgery positively correlate with improved function and pain management post-surgery.
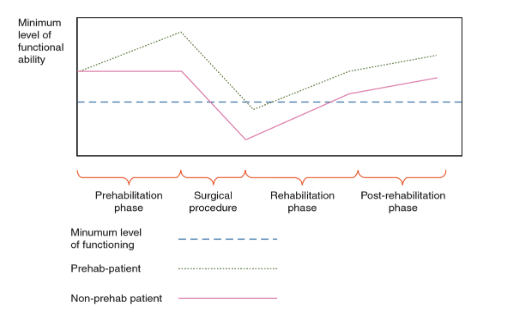 Fig. 1 Model depicting the benefits of Prehabilitation and Post-operative Recovery
Fig. 1 Model depicting the benefits of Prehabilitation and Post-operative Recovery
Cardiac and muscular deconditioning causes the patient to experience a decline in functional capacity. By increasing functional capacity prior to surgery, patients who have completed 6 to 12 weeks of progressive Prehabilitation will retain a higher level of functional capacity postoperatively and return to a minimum level of functional independence sooner compared to non-prehabilitated individuals. The difference in functional capacity post-surgery is attributed to intensity, frequency, duration and compliance of Prehabilitation.
Megan Fraser
Accredited Exercise Physiologist

